Table of Contents
- Introduction
- What Is Healthcare Revenue Cycle Management?
- Core Components of Hospital RCM
- Why Is Healthcare Revenue Cycle Management Important?
- Common Challenges and Errors in the RCM Process
- The Growing Trend of Outsourcing Medical Billing and RCM Solutions
- Advantages of Outsourcing Medical Billing and Healthcare RCM Solutions
- RCM Healthcare: 2026 Trends in Hospital Revenue Cycle Management Solutions
- Selecting an Outsourcing RCM Healthcare Partner
- Frequently Asked Questions (FAQ) – Revenue Cycle Management in Healthcare
1. Introduction
Healthcare Revenue Cycle Management (Healthcare RCM) is the backbone of every successful healthcare organization. In healthcare, RCM in medical billing refers to the entire process of managing financial transactions from patient registration and insurance verification to final payment posting.
It ensures that every clinical encounter is accurately captured, coded, billed, and reimbursed so providers can protect margins, reduce administrative friction, and focus on patient care.
2. What Is Healthcare Revenue Cycle Management?
Revenue Cycle Management (RCM) is the end-to-end financial and administrative framework that follows a patient’s journey from the first point of contact through final claim resolution. It typically includes:
- Capturing accurate demographic and insurance details
- Verifying eligibility and benefits
- Recording charges for all services and supplies
- Applying correct diagnosis and procedure codes
- Submitting clean claims to payers
- Posting payments and managing denials or appeals
The revenue cycle management process links front-end operations like scheduling and registration with back-end functions such as medical billing, coding, and claims submission. When those pieces work together, healthcare organizations can shorten days in A/R, reduce write-offs, and stabilize cash flow.
3. Core Components of Hospital RCM
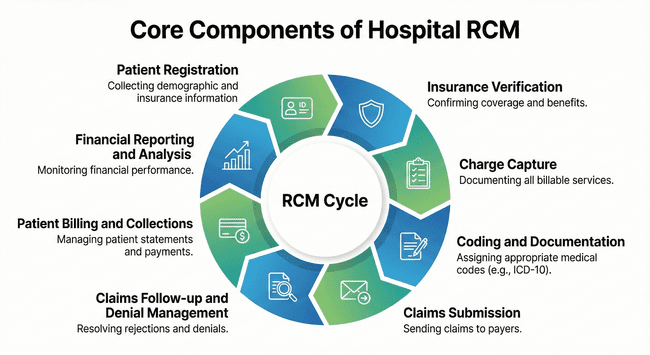
The critical components of hospital RCM typically include the following:
- Patient Registration: Gathering patient demographic and insurance information, verifying eligibility, and establishing financial responsibility.
- Insurance Verification: Verifying insurance coverage, determining pre-authorization requirements, and ensuring accurate billing information.
- Charge Capture: Accurately capturing and documenting all billable services, procedures, and supplies provided to patients.
- Coding and Documentation: Assigning appropriate medical codes (such as ICD-10 and CPT codes) to the patient’s diagnosis and treatment, ensuring compliance with regulatory guidelines.
- Claims Submission: Preparing and submitting accurate insurance claims to the appropriate payers (e.g., insurance companies, government programs) within specified timelines.
- Claims Follow-up and Denial Management: Tracking and resolving claim rejections, denials, or underpayments by investigating errors, submitting appeals, and ensuring proper reimbursement.
- Patient Billing and Collections: Generating patient statements, explaining charges, collecting co-pays, deductibles, and outstanding balances, and managing payment plans or financial assistance programs.
- Financial Reporting and Analysis: Monitoring and analyzing financial performance, identifying trends, and generating reports to evaluate revenue, cash flow, and key performance indicators.
Efficient revenue cycle management is essential for healthcare organizations to optimize revenue, minimize claim rejections and denials, reduce payment delays, and improve overall financial performance. It requires a combination of accurate coding and documentation, effective billing processes, streamlined workflows, and diligent follow-up on claims and patient payments.
Many healthcare providers outsource their revenue cycle management to specialized companies or consultants to ensure proper management of this critical aspect of their business and to focus on delivering quality patient care.
4. Why Is Healthcare Revenue Cycle Management Important?
The importance of RCM in healthcare goes far beyond billing. A strong revenue cycle:
- Protects margins in an environment of shrinking reimbursement and rising costs
- Reduces administrative burden on clinical and back-office teams
- Supports compliance with complex payer and regulatory requirements
- Improves the patient financial experience through accurate, transparent billing
When RCM is managed strategically, it becomes a growth driver, helping providers reinvest in people, technology, and quality of care.
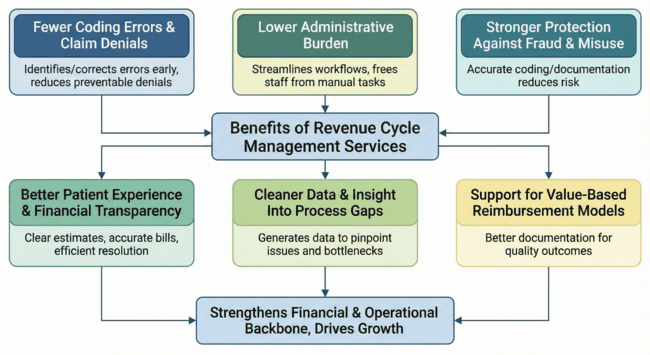
The Benefits of Revenue Cycle Management Services
Effective revenue cycle management services don’t just improve collections – they strengthen the entire financial and operational backbone of a healthcare organization.
- Fewer Coding Errors and Claim Denials
Well-managed RCM helps identify and correct coding and data errors before claims go out the door. This reduces preventable denials caused by incomplete patient information, incorrect CPT/ICD-10 codes, and missed code-set updates. Fewer denials mean faster reimbursements and less time spent on appeals.
- Lower Administrative Burden and More Staff Time for Patients
By streamlining claim workflows, eligibility checks, scheduling, and payment processing, RCM services free teams from repetitive, manual tasks. Staff can shift their focus from chasing denials and fixing errors to supporting providers and delivering a better patient experience.
- Stronger Protection Against Fraud and Misuse
Accurate coding, proper documentation, and tight billing controls help reduce the risk of fraud and abuse, such as upcoding, billing for services not rendered, or unnecessary procedures. Robust RCM processes also support better insurance verification and patient identity checks, helping flag discrepancies and potential medical identity fraud early.
- Better Patient Experience and Financial Transparency
RCM services streamline registration, benefit verification, and financial discussions so patients know what to expect before and after a visit. Clear estimates, accurate bills, and efficient problem resolution build trust and reduce frustration around payments.
- Cleaner Data and Insight Into Process Gaps
Because RCM touches every step of the patient-to-payment journey, it generates valuable data. Analyzing trends in denials, delays, and write-offs helps organizations pinpoint process issues, missing information, or bottlenecks and make targeted improvements.
- Support for Value-Based Reimbursement Models
As healthcare moves toward value-based care, RCM services help organizations align with new reimbursement models. Better documentation, reporting, and performance tracking make it easier to demonstrate quality outcomes and meet payer requirements tied to value rather than volume.
5. Where Errors Can Occur in the Revenue Cycle and How to Prevent Them
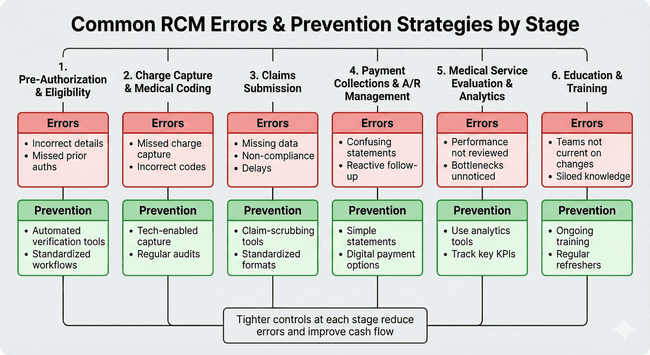
Even well-run organizations face challenges with RCM in medical billing. The most common errors in the RCM cycle tend to cluster around a few key stages. Understanding where these issues occur – and how to prevent them – is essential for protecting revenue and avoiding rework.
Pre-Authorization and Eligibility Verification
Where errors happen:
- Incorrect or outdated insurance details
- Missed prior authorizations
- Incomplete or inaccurate patient demographics
These issues lead directly to claim rejections, delayed payments, and higher write-offs.
How to prevent them:
- Use automated eligibility verification tools at scheduling and check-in
- Standardize front-desk workflows and checklists
- Confirm insurance and demographics at every visit, not just the first
Charge Capture and Medical Coding
Where errors happen:
- Missed or incomplete charge capture
- Incorrect diagnosis or procedure codes
- Insufficient documentation to support coded services
These errors often result in underpayments, denials, or compliance risk.
How to prevent them:
- Implement technology-enabled charge capture integrated with the EHR
- Use computer-assisted coding (CAC) tools where appropriate
- Conduct regular coding audits and documentation reviews
- Provide ongoing education for coders and clinical staff on coding updates
Claims Submission
Where errors happen:
- Claims submitted with missing or inconsistent data
- Non-compliance with payer-specific rules
- Delays in submitting claims within the timely filing limits
How to prevent them:
- Use claim-scrubbing tools to flag errors before submission.
- Standardize formats and workflows for electronic claims (EDI)
- Monitor submission timelines with dashboards and alerts.
- Clear communication of patient responsibility at the front end also reduces downstream billing friction and helps ensure smoother collections.
Payment Collections and A/R Management
Where errors happen:
- Confusing, hard-to-read patient statements
- Lack of convenient payment options
- Reactive, inconsistent follow-up on outstanding balances
How to prevent them:
- Send simple, itemized statements that clearly show what insurance paid and what the patient owes
- Offer digital payment options (online portals, text-to-pay, payment plans)
- Use automated reminders and structured A/R workflows to keep balances from aging out
Medical Service Evaluation and Analytics
Where errors happen:
- Revenue cycle performance is not regularly reviewed
- Bottlenecks and recurring errors go unnoticed
- KPIs like days in A/R, denial rates, and first-pass resolution are not tracked consistently
How to prevent them:
- Use analytics tools to monitor each stage of the revenue cycle
- Track key KPIs and drill down into root causes of recurring issues
- Launch targeted process improvements where data reveals patterns (e.g., a specific payer, code set, or clinic location)
Education and Training Programs
Where errors happen:
- Teams are not kept current on coding changes, payer rules, or new technologies
- Knowledge is siloed, and best practices aren’t shared across departments
How to prevent them:
- Invest in ongoing training for coding, billing, and front-office teams
- Provide regular refreshers when payer or regulatory changes occur
- Use audit results to guide focused coaching and process updates
By tightening controls at each stage from pre-authorization to collections and analytics, healthcare organizations can significantly reduce common errors in the RCM cycle, improve cash flow, and minimize the need for time-consuming investigations and appeals.
6. The Growing trend of Outsourcing Medical Billing and Revenue Cycle Management Solutions
As the healthcare industry becomes more complex, healthcare executives face numerous challenges in managing medical invoicing and revenue cycle management (RCM). Many healthcare providers use outsourced medical billing and RCM solutions to address these challenges. Here are a few reasons:
Staffing Shortages: One major hurdle for medical practices is the need for more qualified personnel in billing and RCM roles. This scarcity leads to longer processing times, errors, and backlogs. Outsourcing medical billing and RCM functions can address these staffing shortages by providing access to a team of experts trained in the latest best practices. These specialized outsourcing partners offer quicker processing times, reduced errors, and efficiency. Inflation: Inflation has significantly impacted medical practices, increasing costs for supplies, equipment, and personnel. Managing billing and RCM in-house becomes challenging for providers trying to maintain profitability. Outsourcing these functions to a third-party provider can reduce expenses and optimize revenue cycle management. Studies show that outsourced medical billing can substantially increase revenue, countering the effects of inflation.
As regulations, payer rules, and patient financial responsibility grow more complex, many organizations are re-evaluating whether RCM is best handled in-house or through a specialist partner. This shift has led to a growing interest in specialized RCM solutions and outsourcing models that combine technology, expertise, and scalability.
RCM Solutions and Outsourcing for Healthcare Providers
In-house RCM offers greater direct control, but it can be difficult to sustain:
- Recruiting and retaining experienced billing and coding staff
- Keeping up with constant payer and regulatory updates
- Investing in modern RCM technology and analytics tools
Outsourced RCM solutions that healthcare providers use combine expert teams with proven workflows and advanced platforms. Leading revenue cycle management companies leverage AI, automation, and data analytics to:
- Scrub claims and predict denials before submission
- Prioritize follow-ups based on recovery potential
- Identify coding and documentation gaps
- Deliver real-time dashboards for executives and RCM leaders
Partnering with experienced revenue cycle management companies like GeBBS enables providers to optimize coding, billing, and denial management with advanced RCM solutions.
7. Advantages of Outsourcing Medical Billing and Healthcare RCM Solutions
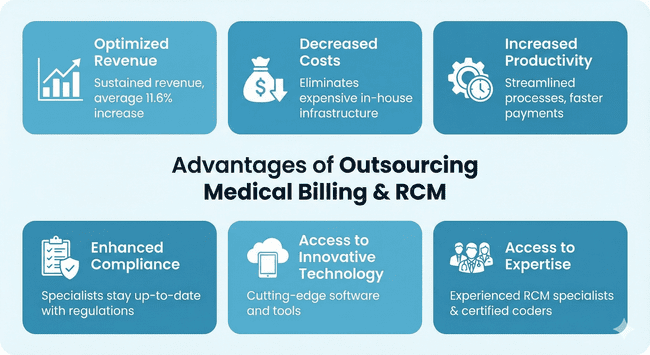
Optimized Revenue: Outsourcing medical invoicing and RCM has significantly sustained revenue for medical practices. Studies indicate that practices outsourcing their invoicing experienced an average increase of 11.6% in revenue. Additionally, collections increased by an average of 6.8%, surpassing the cost of outsourcing and providing an immediate return on investment.
Decreased Costs: Outsourcing eliminates the need for expensive in-house infrastructure, software, and trained personnel. Studies show that billing costs decreased by 16.9% for practices outsourcing their billing functions.
Increased Productivity: Outsourcing medical billing and RCM enables practices to benefit from streamlined processes and expertise. Efficient handling of these tasks leads to faster payments, reduced claim denials, and improved cash flow. It also allows practices to focus more on patient care and critical aspects of their business.
Enhanced Compliance: Keeping up with the complexities of revenue cycle management and compliance requirements can be challenging. Outsourcing ensures that a team of specialists stays up-to-date with the latest regulations, minimizing errors and reducing the risk of audits and penalties.
Access to Innovative Technology: Outsourcing partners invest in the latest software and technology, providing medical practices with access to cutting-edge tools and industry trends that they may be unable to afford independently.
Access to Expertise: Outsourcing RCM in medical billing grants practices with access to a team of experienced professionals, including medical billing and RCM specialists, certified medical coders, and industry thought leaders. These specialists are trained to adhere to regulations and compliance requirements, resulting in faster payments and fewer claim denials.
8. RCM Healthcare: 2026 Trends In Hospital Revenue Cycle Management Solutions
Emerging Trends in Healthcare Revenue Cycle Management
The healthcare revenue cycle management (RCM) market continues to evolve rapidly, driven by technological innovation, increasing patient responsibility, and a greater focus on efficiency and compliance. Below are some of the key trends shaping the future of RCM:
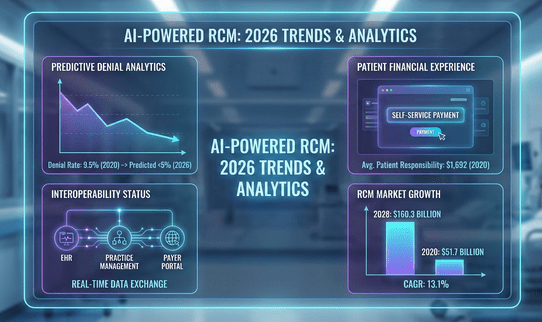
Growing RCM Market: The global healthcare RCM market is experiencing significant growth. According to a report by Grand View Research, the market was valued at USD 51.7 billion in 2020 and is expected to reach USD 160.3 billion by 2028, growing at a compound annual growth rate (CAGR) of 13.1% during the forecast period.
Increased Interoperability: Seamless data exchange between Electronic Health Records (EHR), practice management systems, and payer portals is becoming the norm. This real-time connectivity reduces claim submission errors and accelerates reimbursement cycles. The impact: providers enjoy quicker claim approvals and better denial prevention. Patients benefit from more transparent, accurate billing statements.
Outsourcing Healthcare RCM: Many healthcare providers outsource their RCM processes to specialized companies. This trend is driven by the need to reduce costs, improve operational efficiency, and enhance revenue capture. According to a Black Book Market Research survey, approximately 68% of hospitals with over 150 beds outsourced their RCM functions in 2020.
Importance of Technology — Growth of Predictive Analytics and AI: Technology plays a crucial role in streamlining RCM processes. The past is paper charting. The present and future is charting electronically. Electronic Health Records (EHR) systems, revenue cycle management software, and automation tools help improve accuracy, increase efficiency, and reduce manual errors.
AI-driven tools now predict potential claim denials, highlight coding discrepancies, and optimize payment collection strategies. Healthcare Financial Management Association (HFMA) data from late 2024 reveals that 82% of large health systems have integrated some form of AI in their RCM processes. The impact: by proactively resolving errors, providers reduce denial rates, shorten days in AR, and enhance revenue forecasting for strategic planning.
Focus on Patient Experience: High-deductible health plans remain prevalent, meaning patients shoulder more healthcare costs. Providers are adopting digital front doors and self-service payment portals to improve the billing experience. The impact: engaging patients early and often about out-of-pocket responsibilities reduces unexpected costs and fosters trust. Many organizations report higher patient satisfaction scores and fewer unpaid balances.
Rising Patient Financial Responsibility: With the increase in high-deductible health plans and shifting healthcare costs to patients, healthcare providers face challenges collecting patient payments.
A survey by TransUnion Healthcare revealed that in 2020, the average patient payment responsibility after insurance increased by 11%, reaching $1,692 per patient.
Focus on Denial Management: Denials and claim rejections can significantly impact revenue. Healthcare organizations emphasize denial management strategies to identify and address root causes, reduce denials, and optimize reimbursement.
The American Hospital Association estimated that hospitals’ average claims denial rate was around 9.5% in 2020.
Regulatory Compliance: Compliance with regulatory guidelines, such as HIPAA (Health Insurance Portability and Accountability Act) and ICD-10 coding standards, remains a crucial priority for healthcare organizations. Ensuring accurate coding, documentation, and data privacy protection is vital for RCM success.
These trends and statistics highlight the growing importance of effective revenue cycle management in the healthcare industry. By leveraging technology, outsourcing when appropriate, and adopting best practices, healthcare providers can improve financial performance, enhance patient satisfaction, and streamline revenue cycle processes.
Overall, the future of Healthcare RCM is characterized by continued automation, real-time data analytics, and a greater emphasis on patient engagement. Organizations that remain agile, embrace new technology, and prioritize compliance are best positioned to thrive in this dynamic financial environment.
Selecting an Outsourcing RCM Healthcare Partner
Healthcare RCM remains the linchpin of a provider’s financial health. From front-office tasks like patient registration and insurance verification to back-end responsibilities such as payment posting and denial management, a streamlined RCM process ensures timely reimbursements and sustained revenue growth.
In 2026, Healthcare RCM is more integrated, data-driven, and patient-focused. Providers that prioritize ongoing staff education, adopt robust technologies, and partner with specialized RCM services like GeBBS Healthcare Solutions will be well-prepared to navigate this ever-evolving industry. By staying proactive, organizations can not only safeguard their bottom line but also deliver a superior patient experience that keeps patients returning for quality, reliable care.
Choosing the Right Revenue Cycle Management Partner

Selecting an RCM partner is a strategic decision that directly impacts financial performance, compliance posture, and patient experience. Key criteria to evaluate include:
- Industry experience and compliance expertise
Look for deep healthcare domain knowledge, certified coders, and proven experience with your specialty mix, payer mix, and facility type.
- Transparent reporting and KPIs
Your partner should provide clear SLAs, dashboards, and regular performance reviews that cover metrics like days in A/R, clean-claim rate, denial rate, and net collection ratio.
- Advanced automation technology
Ask about the use of AI, RPA, and analytics, as well as integration capabilities with your EHR, practice management, and clearinghouse platforms.
- Proven track record in reducing denials
Request case studies and references demonstrating success in lowering denials, accelerating reimbursement, and improving cash flow.
GeBBS Healthcare Solutions provides end-to-end RCM services designed to improve accuracy, reduce overhead, and deliver measurable ROI.
Why Partner with GeBBS Healthcare Solutions?

As a leading provider of technology-enabled revenue cycle management services, GeBBS helps hospitals, health systems, and physician groups streamline the entire patient-to-payment journey. We combine deep healthcare domain expertise and HITRUST technology reliability, with modern AI automation such as iCodeOne and analytics to improve collections, reduce denials, and create more predictable revenue cycles.
Recognized as a “Leader” in the Everest Group Revenue Cycle Management (RCM) Operations PEAK Matrix® Assessment and consistently ranked in the IAOP® Global Outsourcing 100 and the Inc. 5000 list, GeBBS brings a proven track record of performance and scalability to its clients.
When choosing an outsourcing revenue cycle management company partner, it is crucial to consider their technology and service expertise with RCM coding, RCM billing, and RCM healthcare outsourcing services. GeBBS Healthcare Solutions provides revenue cycle management solutions tailored to healthcare providers. Our proven track record of optimizing revenue and decreasing payment cycle times for clients is a testament to how we’re one of the most reputable healthcare revenue cycle management companies and medical coding companies in the US!
GeBBS’s technology and service solutions span patient contact, HIM, extended business office, and risk adjustment services, giving providers a single, accountable partner for their end-to-end RCM needs. Backed by rigorous security and compliance frameworks and a global delivery model, GeBBS is focused on delivering measurable financial impact while allowing providers to stay focused on high-quality patient care.
Contact GeBBS Healthcare Solutions today to schedule a consultation and discover how our revenue cycle management solutions can improve accuracy, reduce overhead, and deliver measurable ROI for your organization.
10. FAQ Section
RCM in medical billing refers to the comprehensive financial process that oversees patient revenue. This process encompasses everything from scheduling and verifying patient eligibility to coding, submitting claims, processing payments, and managing collections. The goal is to ensure accurate reimbursements, maintain compliance, and establish consistent cash flow.
The key steps in the RCM cycle include preregistration, registration, charge capture, claim submission, remittance, insurance follow-up, and patient collections. These steps are organized into front-end, mid-cycle, and back-end activities to secure timely reimbursement.
RCM is critical in healthcare because it minimizes billing errors, accelerates the reimbursement process, reduces claim denials, supports compliance, and enhances the patient experience. This, in turn, helps preserve profit margins and ensures access to care amidst various payer requirements.
RCM companies enhance cash flow by optimizing processes such as eligibility verification, coding accuracy, claim submissions, and denial management. They expedite collections, shorten days in accounts receivable (A/R), reduce write-offs, and lower operational costs through automation and expertise.
Important KPIs for RCM that healthcare organizations should monitor include days in accounts receivable, clean claim rate, denial rate, net collection rate, alarming debt rate, and first-pass resolution. Tracking these metrics helps identify bottlenecks and guide improvements in revenue performance.
Prior authorization in RCM refers to the requirement for payer approval before certain services or medications are provided. Inefficient workflows related to prior authorization can lead to delayed care and increased denials. Strong authorization processes protect patient access, reduce the need for rework, and support timely reimbursements.






