Achieving Business Objectives with Effective Coding & Preventable Denial Strategies
I. Introduction
Denials are a leading source of revenue loss and increased labor costs for healthcare organizations. Hospitals across the country lose approximately $262 billion per year on denied claims from insurers, sparking huge cash-flow issues and recovery costs. An estimated 9% of hospital charges are denied every year, putting almost $5 million per hospital at risk.1 Although
there are many contributing factors, coding errors are often at the root of costly denials. While not only is the impact of these denials burdensome, the added costs to identify, correct, and appeal coding denials puts an even greater financial strain on already taxed health systems, especially on coding errors that are mostly avoidable.
II. Identifying the Source of Coding Errors is Critical
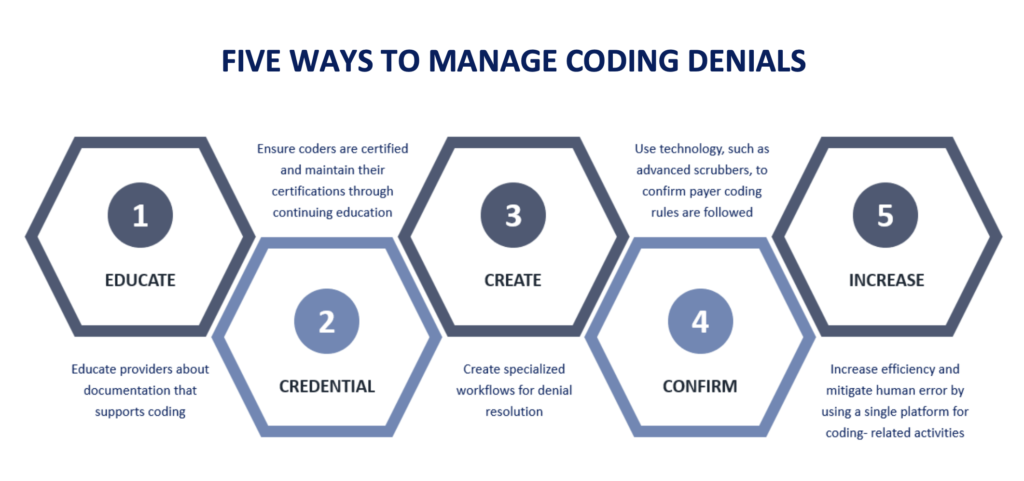
Although the reasons for some denials rests solely on the shoulders of coders, there are varied explanations for incorrect, missing, and/or inappropriate coding. Analysis of denial patterns is an essential first step to locate the source, but it is not enough to rely solely on reports. Experienced, certified coding and revenue cycle professionals can look beyond the numbers to find the true source of coding denials, the majority of which fall into two specific categories: Clinical Error and Coder Error
According to the Office of Inspector General (OIG), best practice is to maintain >95% coding accuracy.
III. Coding Error Source #1: Clinical Error
All diagnosis and procedure coding evidence must be contained within clinician documentation from a specific encounter. Coders should never assume symptoms, diagnoses, or performed procedures. A common coding saying is, “If it’s not documented, it’s not done”, which is also the most compliant route to take as well. If coded claims compared against documentation
cannot pass an audit, it should not be coded or billed as such. Lack of awareness about coding definitions is often the source of inadequate provider documentation. Correct coding depends on the highest level of specificity. If the information for
a code is not included in the documentation from an encounter, a different, frequently “lower” code that satisfies documentation requirements is used instead, leading to fewer RVUs and diminished reimbursement. Best practice is a constant communication flow between coders and clinicians, to ensure everyone is aware of the information needed to assign correct codes,
bill accurately, avoid denials, and keep cash flowing consistently.
Many organizations use clinical staff to submit authorizations for treatment and hospital stays. Approvals usually require diagnosis and procedure codes. Requests with inaccurate information can result in delayed or denied treatment or denied claims after the adjudication process, resulting in time-consuming appeals and often zero reimbursement. According to a recent
survey by the AMA (American Medical Association), almost a quarter of providers said that a prior-authorization delay impacted the health of a patient, with 16% believing the delay led to hospitalization.3 In addition to avoiding denials, clinicians can help expedite required treatment with appropriate coding information on necessary authorization requests.
IV. Coding Error Source #2: Coder Error
Denials from coder error occur when an incorrect diagnosis, treatment, or procedure code is
filed on a claim despite access to accurate documentation.
Coders can make improper choices, often due to lack of education or experience, which
repeatedly leads to a multitude of burdensome denial reasons, such as:
• Medical Necessity
• Diagnosis Sequencing (primary, subsequent, and comorbidities)
• Highest Level of Specificity
• National Coverage Determinations (NCDs)
• Local Coverage Determinations (LCDs)
• National Correct Coding Initiative (NCCI) Edits
• Bundled and Unbundled Codes
• Payer Rules
It is critical to ensure correct coding. The most predominant 20% of CPT codes (usually around 20 – 40 codes) drives 80% or more of revenue for many practices.
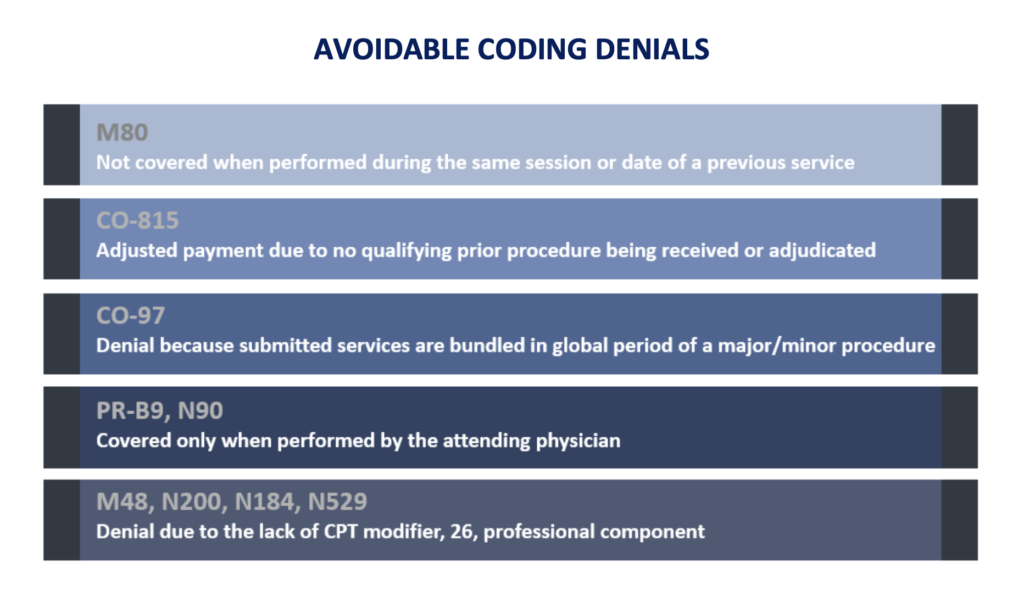
V. Avoiding Common Coder Errors
The building blocks coders use to communicate claims information to payers are diagnosis codes, procedure codes, treatment codes, and modifiers. There are common errors associated within each.
Diagnosis Errors
One of the most common errors is the lack of medical necessity when a diagnosis does not support the procedure or treatment. Frequently, the coder has overlooked the primary diagnosis, chosen the incorrect diagnosis, or failed to report all illness signs and symptoms. The proper selection and sequence of diagnosis codes also plays a vital role in substantiating medical necessity. Primary and secondary diagnoses along with comorbidities, additional bolster the case to ensure claims are appropriately reimbursed in full.
The sequence of procedure coding affects reimbursement. Under multiple procedure payment reduction (MPPR), many payers (including Medicare) can reduce second and subsequent procedure reimbursements by 50% during an encounter
Treatment and Procedure Errors
While diagnosis coding follows ICD-10 rules, outpatient treatment and procedure coding
encompasses two code sets, CPTs and HCPCS. Most commercial payers use CPTs solely, but other payers will use a combination of both CPT and HCPCS – which means even if the correct code for the code set is used, the claim can still deny because of payer rules.
Institutional knowledge is crucial to avoiding these mistakes, as well as identifying how to correct a claim. Continually updating information on NCDs, LCDs, NCCI edits, and code set revisions is essential in remaining compliant and to avoiding denials. Coding updates happen several times a year, and costly mistakes are made when coders are not always kept current or well-informed, not properly educated, and have not regularly maintained valid certification.
The Burden of Applying Correct Medicare Modifiers6
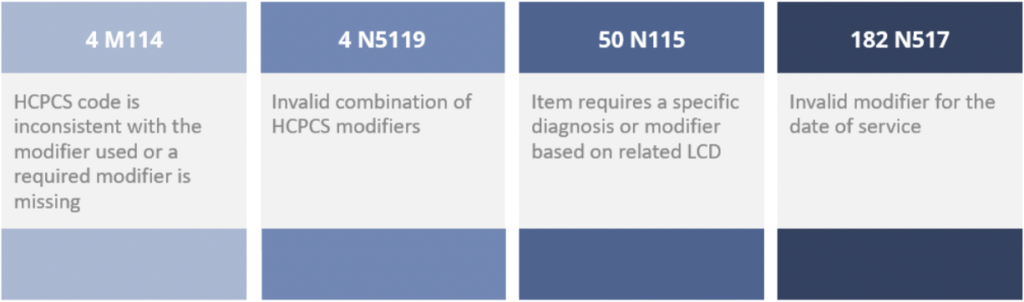
Modifier Errors
Modifiers are designed to communicate additional information about a treatment or procedure and are expressed as two numeric or alphanumeric characters. Modifiers are necessary to offer added and supporting information about the procedures, services, or supplies involved without changing the actual meaning of the code. They describe circumstances that affect procedures
and could potentially impact reimbursement. Both CPT and HCPCS code sets use their own set of modifiers, and as with procedure coding, payers can dictate which type of modifier is used on their claims.

“Coding quality for Medicare claims is an area of constant concern. Coding errors canhave far-reaching effects in the healthcare universe, and coders are experiencingincreased scrutiny from both regulators and hospitals looking to control costs.”7
VI. GeBBS in Action
A Team Approach Decreases Coding Denials to Increase Collections by 19%
A 300-bed facility, known for a stellar cardiothoracic surgery program as well as for its outstanding neurosciences team, approached GeBBS because of its high volume of coding denials. The organization estimated its collections had dipped 22% due to coding inaccuracies, with an additional 6% increase in associated timely filing write-offs. Upon investigation, GeBBS determined several factors contributing to coding errors. Operational issues, provider confusion about appropriate modifiers, correct determination of new versus established patients, lack of specificity during diagnosis coding, and incorrect use of
G-code, all combined, created a denials workload so heavy, that the billing department struggled to submit appeals and simply wrote-off recoverable revenue.
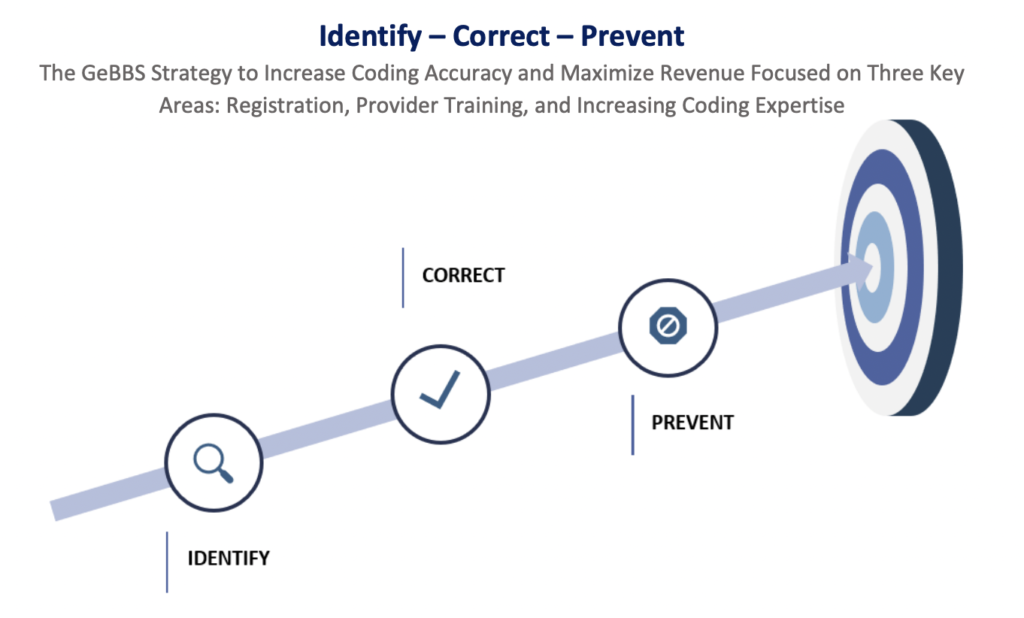
Identifying a Leading Source of Denials – Registration
Many denials stemmed from incorrect patient details and inaccurate insurance information. The GeBBS team analyzed reports to identify staff training opportunities and provided much needed proactive education. The process was reorganized to consistently review quality and to coordinate backup and other support efforts.
Correcting Educational Gaps – Provider Training
GeBBS drafted CPT crosswalks to ensure accurate coding and created detailed documentation guidelines with checklists and matrices to capture relevant details to correct deficiencies. The team routinely audited claims to identify errors and opportunity, including other relevant codes that enforced compliance, while having a positive impact on revenue.
Preventing Unwarranted Denials – Increasing Coding Expertise
The GeBBS team identified a specific area of under-coding for cardiac catheterization and cardiac and thoracic surgery. These claims contributed 20 – 25% of overall claim volumes and significantly impacted collections. Accurately coding to the highest level of specificity reduced diagnosis-related denials and appropriately using XE, XS, LC, LD, and LM modifiers, further lowered denial rates. The GeBBS team also put a robust plan in place to prevent future denials.
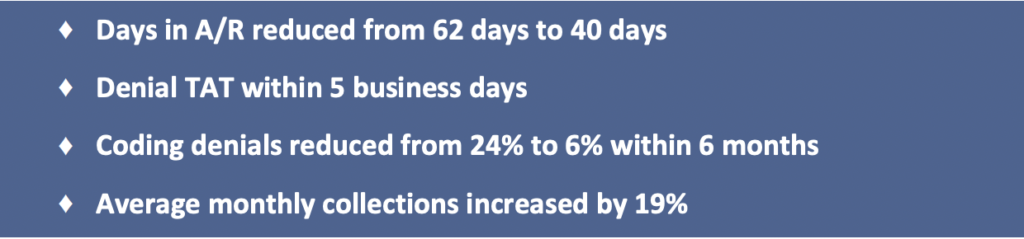
GeBBS Impact
The team’s approach of standardized workflows to monitor claims, quick identification and resolution of new denials, and provider education and communication to prevent future denials, produced marked results and significantly improved performance:
Disparate Systems Can Largely Be Another Source of Coding Denials
A recent survey found 72.5% of responding hospitals that reported having the most trouble with denials were using three or more revenue cycle management systems.8 Signing-in to separate platforms to confirm patient demographics and insurance information, obtain patient records, and review submitted claims and payment information contributes to high labor costs and leaves room for human error. It also highly inhibits the ability to sufficiently audit for quality and provide needed feedback for improvement.

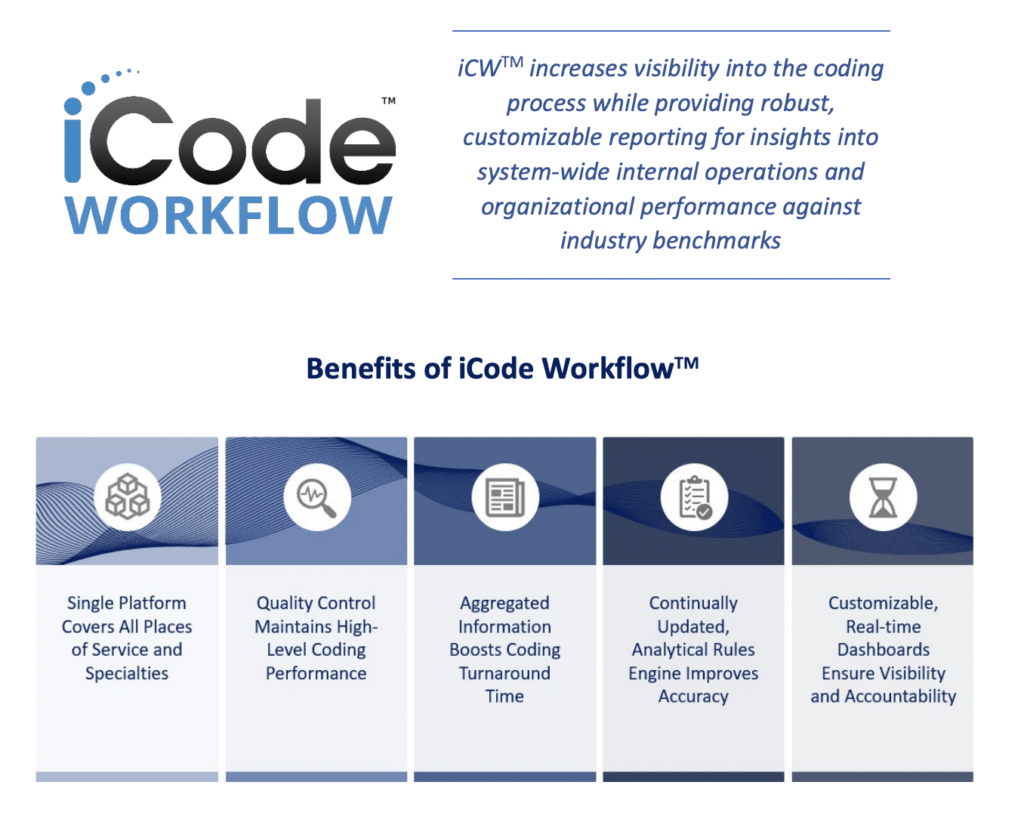
VII. The Solution: iCode Workflow
iCode WorkflowTM (iCWTM) is a single-platform solution that enhances the coding process with intelligent workflows and integrated quality assurance. iCW technology integrates with all EHR and practice management systems directly to consolidate claim and clinical information inputs (including HL7, DOCX, CSV, PDF, and TIFF-scanned paper reports) from each location and
specialty onto a single, secure, cloud-based platform. Real-time dashboards manage production and service levels while coders are monitored with individual metrics and quality scores. iCW’s proprietary rules-based engine supports coding accuracy to optimize efficiency and maximize revenue.
VIII. Operational Focus: Managing High-Volume Denials
Knowledge and experience are the two most important characteristics in solving coding denials. Work queues defined by payer and denial type increase the efficiency and accuracy of denial resolution.
Know the Difference Between Claims That Require Corrections and Coder Review
Specialized teams are adept at understanding the difference between the need for a code correction and when a coder review is appropriate. Coder reviews are often necessary to resolve medical necessity denials and can be time-consuming. Coding corrections do not always require coder intervention because the claim already contains the required information for
successful adjudication.
Experience with Payers
Often claims are not denied outright, and processing is put on hold until records are received and reviewed. In cases like this, addressing the payer’s specific documentation concerns is vital to getting the claim paid. This level of experience increases efficiency when providing relevant documentation and correlating records to prevent impending coding denials.
IX. The GeBBS Advantage
GeBBS Healthcare Solutions is a KLAS rated leading provider of technology-enabled Revenue Cycle Management (RCM) services and solutions in Health Information Management (HIM), Accounts Receivable (A/R) and Risk Adjustment outsourcing. GeBBS’ innovative technology, combined with its over 9,500-strong global workforce, helps clients improve financial performance, adhere to compliance, and enhance the patient experience. Headquartered in Los Angeles, CA, GeBBS has won numerous accolades for its medical coding and medical billing outsourcing, including being ranked in Modern Healthcare’s Top 10 Largest RCM Firms, Black Book Market Research’s Top 20 RCM Outsourcing Services, and Inc. 5000’s Fastest Growing Private Companies in the US.
It is time to see what GeBBS Healthcare Solutions can do for your organization?
Contact us today at 888-539-4282 to see how we can assist you with your RCM operations or Request a Consultation with one of our solutions experts.
References
- Barkholz, D. (2017, June 27). Insurance claim denials cost hospitals $262 billion annually.
Retrieved from
https://www.modernhealthcare.com/article/20170627/NEWS/170629905/insurance-claimdenials-cost-hospitals-262-billion-annually - Department of Health and Human Services. (2000, October 5). OIG Compliance Program for
Individual and Small Group Physician Practices. Retrieved from
https://oig.hhs.gov/authorities/docs/physician.pdf - HealthPayerIntelligence. (2020, June 23). AMA: Payers Did Not Fix Prior Authorization, Cut
Provider Burden. Retrieved from
https://healthpayerintelligence.com/news/ama-payers-did-not-fix-prior-authorization-cutprovider-burden - Selbst, S., & Charkin, S. E. (2015). Managed Care Contracting and Reimbursement. The Journal
of the Healthcare Billing and Management Association, 20(September.October), 11-14.
https://www.sourcenet-usa.com/pdfs/HBMA-Billing-Journal.pdf - Verhovshek, J. (2018, April 05). Just the Facts: Multiple Procedure Payment Reductions (MPPR).
Retrieved from https://www.aapc.com/blog/41773-mppr-facts/ - Denial Code Resolution – JD DME – Noridian. (2020, February 6). Retrieved from
https://med.noridianmedicare.com/web/jddme/topics/ra/denial-resolution - Carlton, C (2000, September). Medicare Data Study Spotlights Coding Errors. Retrieved from
https://library.ahima.org/doc?oid=58154#.X6xbr8hKhPY - Miliard, M. (2018, May 7). It’s not just EHRs: Interoperability also poses big challenges for
revenue cycle. Retrieved from
https://www.healthcarefinancenews.com/news/its-not-just-ehrs-interoperability-also-posesbig-challenges-revenue-cycle